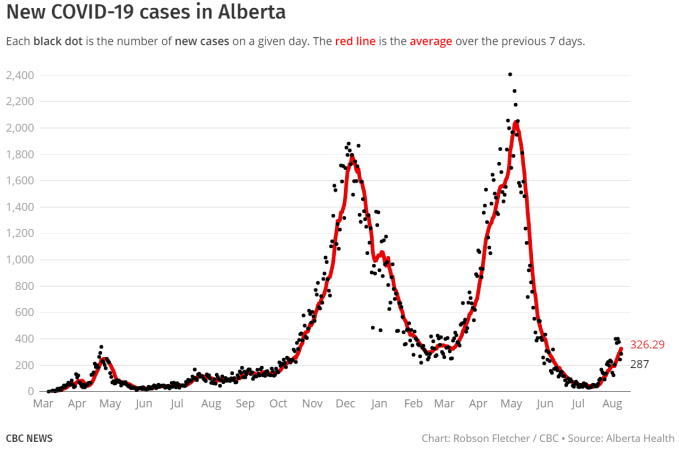
Full disclosure, I am not a statistician, mathematician, nor do I have any special training in statistical modelling, forecasting or epidemiology. However, I have been following the pandemic closely both personally and professionally, and like to look at patterns to see what’s next. As we find ourselves in an early 4th COVID wave in Alberta, driven by the delta variant, our province is set to eliminate all mandatory isolation for positive cases, contact tracing, any provincial mask mandates, and embark on a course of “living with COVID” and carrying on as normal.
I would love to carry on as normal, wouldn’t you? The proposed approach is very reasonable when dealing with an endemic disease to which most of the population carries reasonable immunity, or does not spread too rapidly. By definition, an endemic is a disease that exists at a steady case rate, without significant case increases or outbreaks. See here if you want more nuance. With ongoing spikes and drops in cases, we are clearly still having ongoing outbreaks, which by definition is an epidemic (or a pandemic if it is worldwide).
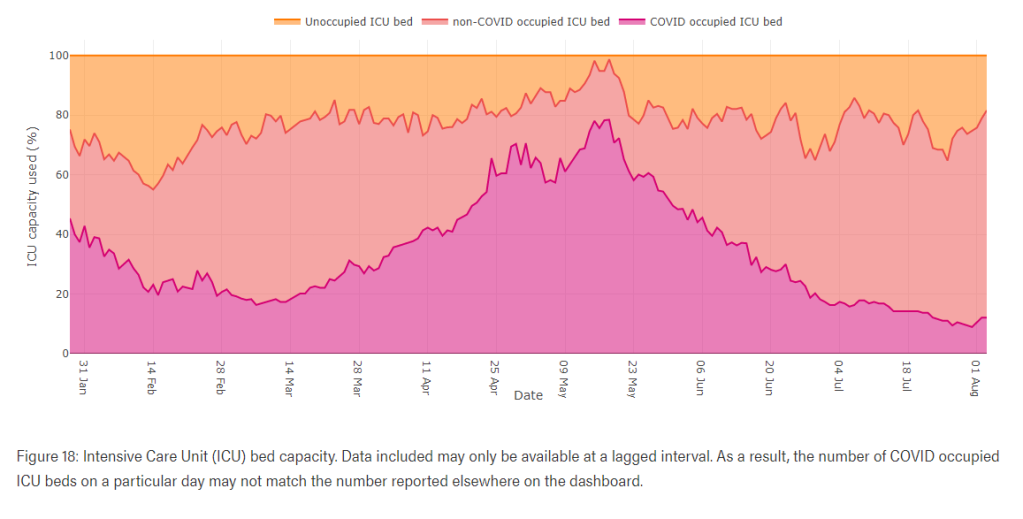
I wanted to do something simple here- try to get an idea from the numbers how at risk our health care system is from the next wave of COVID-19. Alberta has tracked COVID-19 cases and severe outcomes throughout the pandemic. The gathered data is very reflective of what our experience has been thus far. Our rates of severe outcome by age group have been very consistent with other high income countries around the world. If nothing changes, they can accurately predict future observations. However, things have been changing. We now have a good proportion of Albertan’s immunized against COVID-19. As of writing this, Alberta’s COVID website indicates 56.5% of our population is fully vaccinated with 2 doses (We are at 76.2% of “eligible” population with at least one dose, but ineligible children still count as part of the population, and only having a single dose is not fully protective). Those willing to accept a vaccination have now had ample opportunity, and in general children have much less severe disease and far fewer serious outcomes. Our more vulnerable older populations have the highest rates of vaccination. That, along with the economic cost of continuing to trace and isolate COVID cases, appears to be the primary rational given for no longer carrying on with universal pandemic tracking and mitigation measures. A primary purpose of these measures over the last 16 months has been to prevent overwhelming the acute health care system, as that would greatly increase the risk of substandard care both for pandemic patients, and everyone else needing the health care system. Despite over a year of living very restricted lives, with significant and intrusive public health restrictions to slow the spread, Alberta’s ICU system was still strained, and had to be bumped up above regular capacity to handle the case load. At previous pandemic peaks, COVID cases made up a significant portion of ICU capacity.
There are two main reasons to be vaccinated: one is to protect yourself. The second is to protect others by slowing or halting community spread. That’s the same thing we previously did by masking, not gathering and isolating. But with a highly effective vaccine, or effective pre-existing natural immunity, your immune system does that work for you. The SARS COV-2 virus is prone to mutation, which is why we have been dealing with a constant stream of variants. Each one is a subtly new disease. Pre-existing immunity to an earlier strain, either by vaccine or infection can offer partial or full protection against new variants, depending on how recognizable the new variant is to your immune memory. If the immune system is able to quickly identify and kill it, you are unlikely to have much virus replicating in your body, or suffer any symptoms of an infection. If the virus has changed enough that the proteins your immune system is watching for are no longer recognizable, it may behave like a completely new virus, resulting in re-infection needing a new immune response from scratch. This is typical of the seasonal changes of influenza, and the many fast evolving cold viruses. Or the changes may fall somewhere in between – in this case, the virus may be different enough to start an early infection while your immune system adapts to recognize a vaguely familiar foe. Alternately, if the new strain replicates very quickly and your immune system is in stand-by mode, it may be able to infect a lot of cells before your immune memory can be kicked into high gear to start making antibodies to clear it. Either of these scenarios can result in a situation where you can be infected (or re-infected) with the virus, develop symptoms and become contagious. The good news is that in this situation it does not take as long for the immune system to gain the upper hand, and both symptomatic and contagious periods are shorter and less severe.
This is what is happening around the world with the delta strain. A great summary of the latest research on vaccine effectiveness, protection from the delta variant and it’s implications can be found on this blog (by an actual epidemiologist). The short version is that more and more evidence suggests that being fully vaccinated provides good protection against developing symptomatic disease, and excellent protection against severe disease (including hospitalization and death). Below is US data.
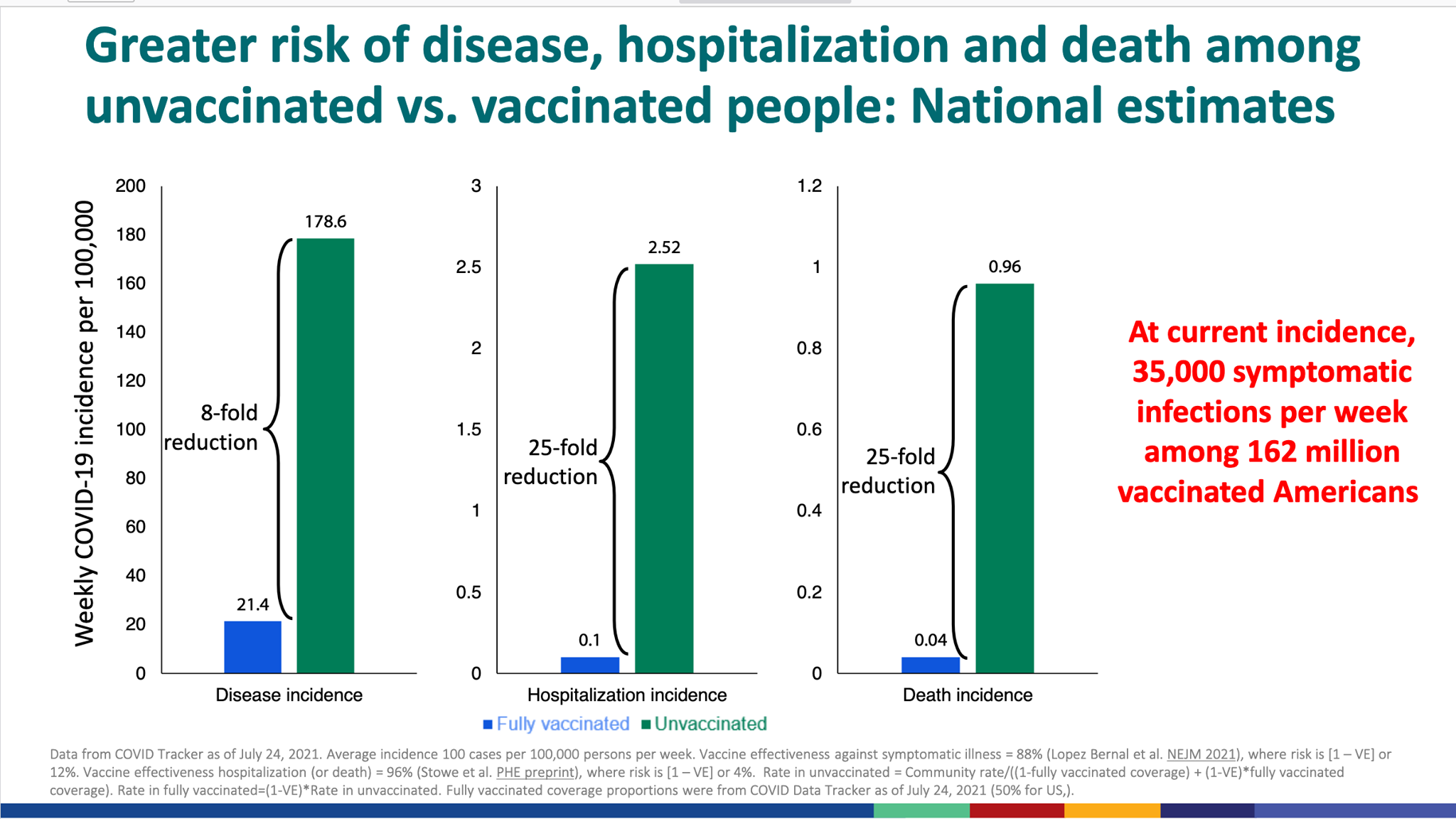
The bad news is that data continues to suggest higher rates of breakthrough cases than previously anticipated (meaning vaccinated people may still have low grade infections and spread the virus to others). So, while vaccines still give personal protection, that community benefit (herd immunity) is likely to be significantly weaker with the delta strain than we had hoped. Good details on this can be found on the above linked blog. This is bad news for the at-risk unvaccinated, and bad news for health care systems that still depend on sick COVID patients not showing up all at once.
What might is look like in Alberta?
This brings me to the crux of this post: Given past trends in hospitalizations and ICU admissions, what kind of numbers might our health care system be looking at if most of our unvaccinated population does become infected with COVID-19 in a very short period of time? This is an important question given that:
1- We have never yet allowed COVID to circulate without public health measures to slow or stop it.
2- Despite high immunization rates in our at risk population, protective herd immunity will likely be lower than normally expected at our current vaccination rate. This means the unvaccinated are at high risk of exposure.
3- The delta variant is proving to be significantly more infectious than previous strains of COVID. Viral loads are about 1,000 times higher than other strains, making it more likely to be passed on in close proximity. The CDC now estimates a single case may infect 8-10 other people, making it one of the most easily spread infectious diseases we know about. This, and the breakthrough transmission through the vaccinated, is behind their latest recommendations to reinstitute universal indoor masking for all.
The Exercise:
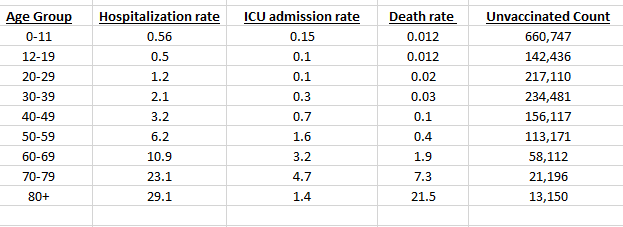
While this is not a scientifically rigorous modelling method, here’s what I did: I took all my numbers from the alberta.ca COVID statistics pages. I took the numbers off this table to see what our Alberta case rates for hospitalizations, ICU admissions and deaths have been in each age category up to this point:
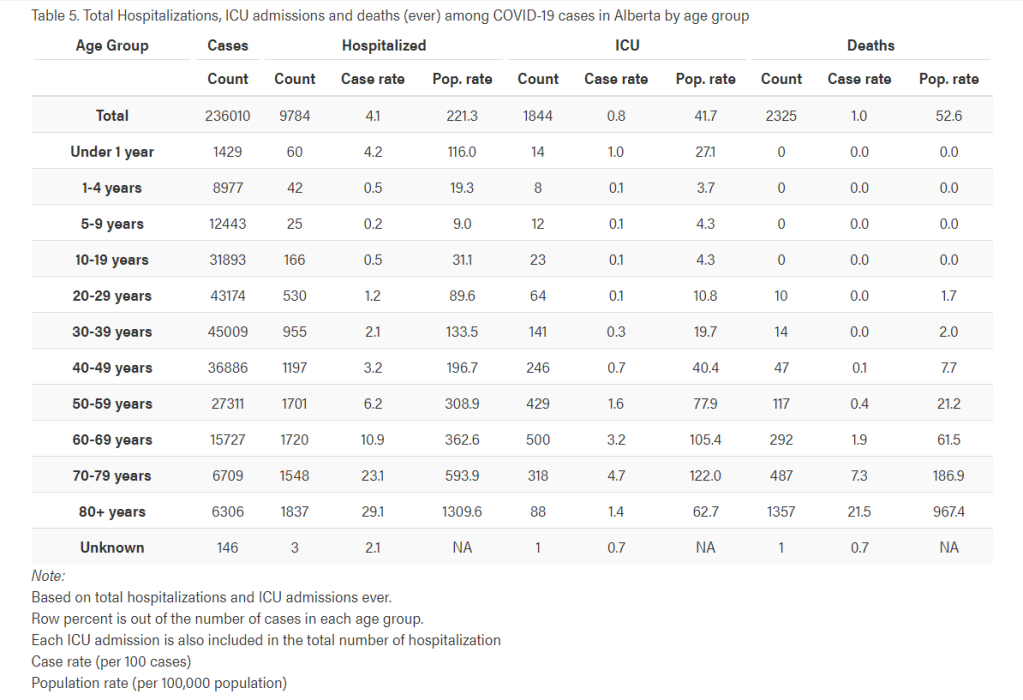
I then used the data on vaccinations by age group from this table, to calculate how many unvaccinated Albertans there are in each age group.

Using the above data, I created the below table in a spreadsheet. A few caveats – in the pediatric population the vaccine and severe outcome age groups do not fully align with one another. For the 0-11 hospitalization and ICU rates, I used the raw numbers to calculate an average for the group (0.56% hospitalized, 0.15% ICU). The actual rates are slightly higher for neonates, and slightly lower for older kids. 12-19 severe rates are based on the reported 10-19 year old rates. Alberta has reported no direct COVID deaths in the 0-19 age group. In order to find a reasonable estimated death rate in the pediatric group, I used this study, which estimated a worldwide pediatric death rate in high income countries of 0.012%. Applying this case mortality rate to our current total of 0-9 year old COVID cases predicts 1.4 deaths, so not having observed one yet is consistent with that rate. Note this study’s pediatric ICU rate was 0.152%, which is not far off Alberta’s observed ICU admission rate of 0.1%.
Next is the simple (ha ha) matter of estimating how many unvaccinated people are going to contract COVID-19 in the coming months, then applying the case hospitalization, ICU admission and death rates to see how much more burden we can anticipate on our system. Now, estimating this properly falls in the domain of professional modelling and statistics, in which I claim no expertise. Yet it seems to me that since we have a disease as transmissible as chicken pox, without mitigation measures, that can spread through some of the vaccinated, with a completely unvaccinated pediatric population that is going to be mingling very heavily in the fall, that a significant percentage of these people are likely to be infected before the end of the year.
Now before moving on, I want to point out some significant limitations to these crude estimates. They come in two categories.
Reasons the numbers might be higher than this estimate:
- I am not including any severe cases in the vaccinated. Although they are rare, there will likely be some.
- I am not including the partially vaccinated (one dose only). That totals about 330,000 people. Although they may have some protection from a single does, we know it is poor protection against the delta strain. I do not have data to estimate severe outcomes in this group. Hopefully it represents people on the way to full coverage.
- I am assuming the same rate of severity for the delta strain as previous strains. We don’t know for sure if that is the case. Online statements by providers from hard hit parts of the US suggest severe outcomes may be more common in both younger, healthier adults, and in children, but I am not aware of reliable data to make an estimate. It’s hard to know if they are seeing a higher rate of severe illness, or simply more severe cases as more people are being infected.
Reasons the numbers might be lower than this estimate:
- I am not accounting for pre-existing natural immunity. While breakthrough cases in former COVID patients are known to happen (and even more with delta), there will be some protection from natural immunity both from re-infection and severe disease. I don’t have a way to account for that, or for knowing how many of the unvaccinated have previous exposure.
- We almost certainly have higher levels of natural immunity than we know. Case counts are always under-estimates of the actual number of infections. There are more people protected by previous infections than will be suggested by past case counts.
- By the same token, the actual case-rates of severe disease are almost certainly lower than those reported, due to the volume of non-reported cases. Applying the reported infection rates onto a full population are going to over-estimate severe outcomes for that reason.
- Behavior changes. Regardless of official regulations, people will often look to protect themselves and others, changing behaviors when it is clear case counts are high in their community. We’ve all had lots of recent practice at these behaviors. Many businesses and perhaps school boards will also mandate their own protections. These measures will help slow spread where they are used.
With all those caveats in mind (and I’m sure more I’ve missed), here are a few screen shots of the calculated rates of severe outcomes at a few wildly different assumptions about the future infection rate solely amongst unvaccinated Albertans. Each age group is using it’s own historical rate and current unvaccinated count in the calculation. Each table contains the actual pandemic to date counts at the bottom for comparison.
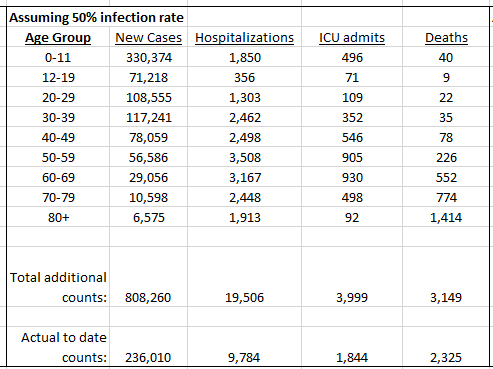
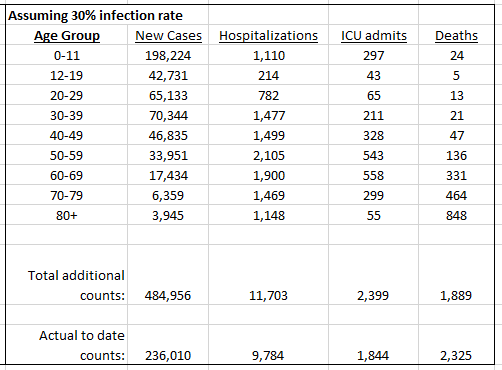
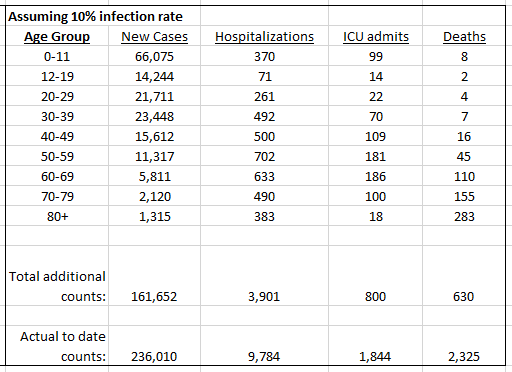
The highest rate I’ve chosen to post is 50%, which one might feel is low in a completely “open for business” world, but I believe my list of caveats in the “numbers may be lower” section will probably have a significant impact on actual future observations. Still, even assuming only 30% of unvaccinated Albertans contract COVID in the coming months, that could almost double our past total COVID ICU admissions. Although kids have low rates of severe outcomes, there are so many that are unvaccinated (all of them), that it is inevitable to see large numbers of hospitalized, severely ill children in completely uncontrolled pandemic spread. We only have 2 hospitals in Alberta with general pediatric intensive care units.
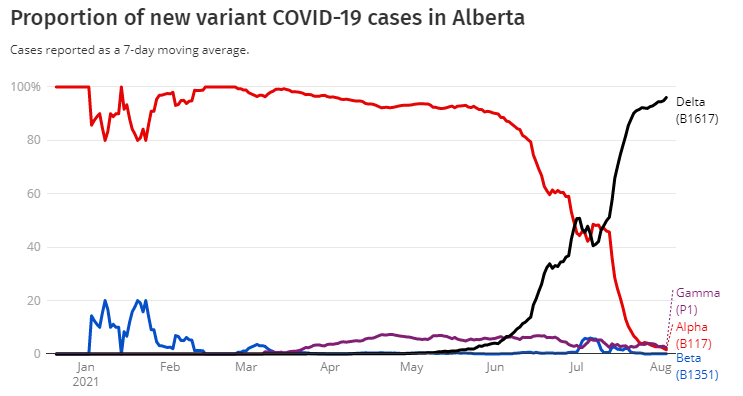
The purpose of this post is not to try and make an accurate future projection, but to point out that even with relatively high vaccination rates (compared to the southern US), we have the potential to still have enough sick, unvaccinated people in a short period of time to cause a significant strain on the health care system. Many US states are now quickly surpassing their peak hospitalization numbers from previous pandemic waves. This is the delta strain that is now dominant in Alberta, as shown in the chart below:
During previous COVID waves, there was a dramatic drop in routine hospital and ER utilization. Cancelled surgeries, people avoiding or delaying coming to hospital for routine issues, and the general full stop to all common respiratory infections cleared space to care for pandemic patients. Hospitals are now very much back to business as usual, and then some. It is an extremely busy summer in most Alberta ERs, and that is with very few serious COVID infections. Hospital capacity in our system is strained at the best of times. This is not the best of times. We are are playing pandemic catch up, providers are burned out, and some places are losing both hospital staff and community providers at an alarming rate. Burn out (the pandemic has been very rough on the health care field), ongoing political confrontation, and the feeling of suddenly having all support for our efforts to keep the pandemic under control swept out from under us is demoralizing for health care providers. On top of all this, there is a real risk that we haven’t yet seen the peak of pandemic demand on the health care system. If many sick COVID patients begin coming in quickly again, we have very little capacity (space and people) to manage it.
It doesn’t have to be that way. The vaccines are providing immense protection (and peace of mind). We don’t need or want to have another lock down. Everyone wants to move on with life, and especially to let our kids be kids. But sticking our heads in the sand won’t make that happen. This is not a call to fear or lock down, but it is a message of concern and caution. Isolating positive cases, testing, tracing and controlling local outbreaks remains essential. They have always been the mainstay for controlling pandemic and epidemic outbreaks. We can’t abandon them now of all times.
Without basic mitigation, we still risk overwhelming the health care system. That means more cancelled surgeries, more delayed cancer diagnoses, longer waits in crowded ERs, and the risk of worse outcomes for any medical condition requiring critical medical care. Too much strain on the system risks making another lockdown the only way to quickly rescue it. Nobody wants that! There are many other small things we can do that may be inconvenient, but still allow us to work, travel, visit and learn in relative safety. We can be cautious a little bit longer until our kids can be vaccinated, protecting them and the greater community. We can live with COVID best by respecting what it is, and acting appropriately. Masks work and remain appropriate in many circumstances. They do not cause harm. If you are not vaccinated, please know that widespread vaccination is the only long term path out of the pandemic. Every time we let infections burn through a community, we increase the chances of yet another variant arising and throwing a monkey wrench in our COVID exit plans. Do it for your community, and perhaps more importantly for yourself. The vaccinations of others are not going to protect you much. A rapidly evolving virus is capable of having different mortality rates each time it comes around, so don’t hang your hat on having been “low risk” one year ago.
The economic and resource cost of pandemic testing and tracing has been put forward as a primary reason to abandon it. I don’t know what a testing center costs, but I do know that an average COVID-19 ICU admission costs $28,000 to our health care system. How many of those can we avoid if we keep up at least the bare minimum of pandemic control measures? How much does it cost to support an infected worker to stay home for a week if it prevents a couple of hospitalizations down the road? When the testing centers are closed at the height of exponential delta spread, how many people will come to the ER for a test when they can’t get one anywhere else? That costs our system several hundred dollars per visit, and I’m sorry to say an over-crowded ER waiting room is not well equipped to keep virus from circulating in the air. As in every part of health care, prevention is always orders of magnitude cheaper than trying to keep people alive when they are seriously ill. Why are we ignoring that fiscal reality?
My colleagues and I are tired of this pandemic, and tired of speaking out. I have heard much more concern privately at Alberta’s new direction than I have publicly, because speaking out into the ocean of pandemic fatigue feels futile. Provincial health policy sounds increasingly like politics and less like science with every new announcement. The constant online environment of medical misinformation takes it toll too. You might not hear from your “medical heroes” of last year as much anymore, but if you look for us, you’ll find us at work, wearing masks, isolating sick patients, washing our hands, and doing most of the same things we have for the past year, while still finding time and space to treat all the other health problems that haven’t gone away. There’s a middle ground between shutting it all down and doing nothing. Can we at least keep up the bare minimum so we don’t have to swing back and forth between those two extremes again?
(Header image source: https://www.cbc.ca/news/canada/calgary/alberta-covid-19-data-statistics-numbers-cases-hospitalizations-1.5514947 Aug 10 2021.