Here we are about a year into the COVID-19 pandemic, and amidst the deluge of statistics, warnings, changing guidelines, protests, conspiracy theories and the continued disruption of our lives, I don’t think everyone feels like they are “in the same boat” anymore. And why would we? The pandemic experience has been different for everybody, and pleasant for nobody. We have all experienced it through the unique lens of our personal experience, personal belief systems, media preferences, and view of the consequences from wherever we are personally standing. With that in mind, I would like to acknowledge the common ground we still share. Whatever your opinion on lockdowns, masks, protests, freedom, public health, economic policy, vaccinations, government competence and overreach, let’s take a moment to agree that this whole experience sucks, and no one likes it.
Think of all the things you miss from late 2019- the changes that make you sad or angry, the things you can’t do and are missing, the people you can’t see because of safety, restrictions, or because they are gone. The losses of income, opportunity and experience are real. Kids are missing out on milestones in their lives, and friends and families are isolated from one another like never before in most of our lifetimes. I feel confident in saying that the person on the other side of the political aisle, the confrontation at the grocery store, or the stranger in the online debate is almost certainly missing the exact same things. Human beings do not thrive in isolation, families cannot succeed in continual economic turmoil, and communities cannot experience normalcy when an invisible deadly threat can strike us or a loved one from a friend or stranger without warning. I think we deserve to give ourselves and those around us a healthy helping of empathy and understanding.
This does not mean we need to accept misinformation, or irresponsible and selfish behavior. It also does not demand a blind and unquestioning acceptance of every decree of government or health authorities. It does ask us to start our questions and our discussions from a place of mutual understanding and respect for the experience and perspective of another. If you do not own a small business that is failing and are at risk of losing your house, then recognize you may not be as intimately aware of the crushing economic consequences of shutdowns as someone who is. If you have not lost one or more loved ones to a sudden and unexpected death with little chance to say goodbye, consider that you might not be able to appreciate the danger and personal anguish of the pandemic as much as someone who has. If you do not work in a hospital or care facility where you see and care for some of the many people suffering and dying from severe Covid-19 infections, your internet-informed musings questioning the reality of the pandemic probably make your entire opinion irrelevant to someone who does. If you have the financial security to enable you to self isolate when sick or exposed without risking loosing your job or the ability to feed your family, then you might not appreciate the terrible choice facing those who risk the possibility of loosing everything when filling out a “fit for work” form when they might not be.
We like our world to be good versus evil, obvious wrong versus obvious right; Luke Skywalker vs the Empire. But real world scenarios are seldom that straightforward, and this pandemic is a perfect example. We (as individuals and as a society) often do not have complete information when making decisions. Especially when it comes to rapidly developing and implementing policies to combat a new and fast spreading infectious disease. Even the experts do not have perfect information, and have been learning as they go. You have heard changing and sometimes conflicting recommendations from health experts through the course of the pandemic. This is because scientific recommendations evolve as new and better information becomes available. When we start off knowing little and learn quickly, what looks to be the best approach is going to change often and quickly. When it comes to scientific advancement, this is in fact “The Way.” And it works. As one example, continuous study and changes in medical practice based on new data in several areas of care have increased the odds of survival in hospitalized COVID-19 patients since the early days of the pandemic. The modern world is awash in information, and no one can be an expert in everything; but as in all complex fields of work and study, the experts still know a lot more than the rest of us do, and we need that expertise. Did you know that the genetic sequence of the COVID-19 causing virus was entirely decoded as early as January 2020? Or that the first prototype mRNA vaccine was developed in a single week-end in that same month? We owe the unprecedented pace of development of current vaccines in part to the experts who were already trying to solve the end game of this pandemic before most people in the world had even heard the word “coronavirus.”
But of course, eventually everyone did hear about the coronavirus, and soon enough could hear about little else. And it goes on. Everyone’s life in one way or another has been turned upside down by something invisible that can only be studied by biological and statistical methods that most people know nothing about, or have only heard about on an episode of CSI. People do not like to lose control of their own lives, especially without understanding why. If the answers were complicated and slow to be found for the experts, is it any wonder people have reached for simple explanations that are easy to understand? There has been an explosion in online commentary on the nuances of PCR cycle counts, infection case definitions, antibody testing, false positives, comorbid diseases, R-values, aerosolization, and a host of other biological and medical terminology that many of these commentators are unlikely to have ever discussed or even hear of before 2020. A few months of online curiosity cannot replace the years of academic background needed to appropriately synthesize and use this information to make and evaluate complex decisions. However, it is often enough to provide a semblance of understanding that feels sturdy enough to support a scaffold of suppositions and inferences that allow someone to explain to themselves what might “really” be happening. In this way one can regain some of that lost sense of control by feeling they can see through the apparent chaos around them, and anchor to an explanation that fits the paradigm of their core belief systems. Often these paradigms cannot fully explain the current reality without the addition of outside interference by someone who is secretly in control, perhaps with sinister motivations that can explain the apparently irrational or overblown responses to the problem. Such ideas often lead to significant suspicion of political or scientific authority figures, or even full blown conspiracy theories.
I do not intend to directly address or challenge every doubt or conspiracy theory, but rather to provide some simple descriptions of some of the unique features of the virus behind the COIVD-19 pandemic. By understanding what makes this virus different than other ones we routinely face, it is much easier to understand why different health organizations and governments around the world have been pushed towards the similar policies and restrictions that have defined our 2020 and early 2021 experience. They are a direct reaction to the nature of this pandemic, and do not require the addition of sinister or conspiratorial motivations to understand how we got here. My intent is not to defend or critique the details of what governments and public health authorities have or have not done, because it has been far from perfect, and is of course colored by political motivations. In fact, I echo the sentiments in this very long article suggesting that if governments were less paternalistic (or conversely dismissive) about COVID restrictions, and more openly communicative about the specific challenges we face and our options to respond, we may have achieved greater cooperative action, and less of the confusion and chaos that has been a breeding ground for suspicion and protest. Understanding the reality of this viruses behavior can better equip us to have the necessary discussion about how to best continue to live with it in the coming months. It is perfectly acceptable and important to discuss the unfortunate trade-offs between public safety, individual freedom and economic security we continue to be faced with, and where it is best to draw the lines. However, this conversation cannot possibly bear fruit unless we understand and accept the same facts, and do not allow them to be overshadowed by fanciful or fearful imaginings of the ulterior motivations we falsely ascribe to others, or wishful thinking about the reality of the virus itself. To use a related medical analogy, you can’t have an open and trusting conversation with your surgeon about treating your life threatening illness if you secretly worry he or she stands to personally benefit from your death and is trying to trick you into making the wrong decision.
As a disclaimer, I am not a virologist or an epidemiologist. I am an emergency department physician with a decent background scientific education and certainly an above average “hobby” interest in immunology and virology, but without credentials in those fields. I have paid close attention to the pandemic, including learning from many better educated in the field. I have treated patients who have suffered and died from COVID-19, and I have also sat around in an empty ER that people were afraid to come to when in retrospect there was little to no COVID-19 circulating in my community. I have tried to pay attention to how the pandemic and it’s societal disruptions have affected those around me, and have thought a lot about why people have come to some vastly different but equally passionate opinions about it and how we have either done too much, or too little to respond. I have become convinced that although opinions will always differ, appreciating the harsh reality of the virus, and acknowledging both the harms of infection and the efforts to limit its spread can open much more productive discussion and solutions.
THE FACE OF THE ENEMY
SARS-CoV-2 (the official name of the virus causing COVID-19 infection) is somewhat of a perfect storm to disrupt modern life. There are a couple of simple reasons for that.
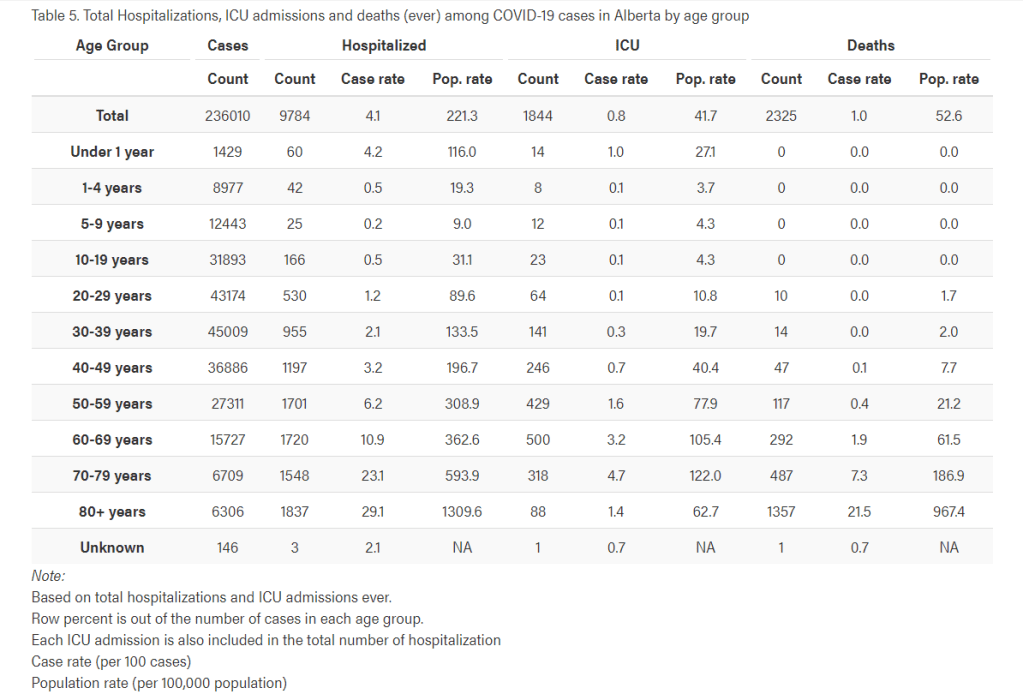
1- It is significantly more deadly than our usually circulating and easily spread viruses. Yes, it absolutely has a higher mortality than the seasonal flu and similar respiratory viruses. I’m not here to convince you of that if you don’t believe it, but there are many good sources to do so with facts instead of media hype (see below for a small sampling). When it enters a particularly vulnerable population, it can cause very high mortality in that group.
2- Infections are mild in most people (about 80%), and completely asymptomatic in some (probably 15-20%). The fact that it is so mild in so many people is what makes it so insidious and has brought us where we are. It is absolutely true that most people who contract COVID will be just fine. This can still be true even with a higher overall mortality. If airplanes had a flawed design by which 1 or 2 out of every 100 passengers died of altitude sickness, most air travelers might still be fine, but the risk of death when flying would still be dramatically higher than it is otherwise.
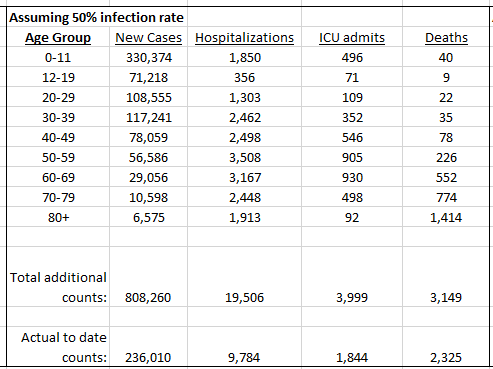
3- COVID-19 is more transmissible than similar respiratory viruses. This means that with normal human day to day behavior, a single infected individual will infect more people than they would with a simple cold or influenza virus. On average, one case of influenza in the general public will infect 1.3 new people. A SARS-CoV-2 case probably leads to 2- 3.5 additional cases (in the absence of infection control measures). This infections per case rate is loosely what is meant when you hear reference to an R-value, although the term and its variations have not always been properly applied in public usage. If you have a hard time visualizing that, draw it out on paper. One person infects 2. Then they each infect 2. Draw that happening 4 times. Then do it again if each person infects 3 others and see how those totals compare after 4 cycles. At each step that gap grows greater and greater. This is exponential spread. On a population scale, this is why fractional increases in seemingly low infection attack rates (R values of 1.5 vs 1.9 for example) can translate into such enormous population effects, and why personal behavior patterns and public health measures that can reduce the current R value can have such a significant effect.
4- COVID-19 has a long incubation period and significant period of asymptomatic infectivity. It is a stealth virus. It commonly takes 5-10, and even up to 14 days to develop symptoms after being infected. And there is a period of time (probably 2 days) before you feel sick (if you ever do) when you can spread it unknowingly to others. In the absence of very intentional and careful surveillance, this allows it to silently spread very extensively in a community for 2-4 weeks (or perhaps longer) before we start to see a significant number of people actually becoming very unwell. Once it is detected in the form of a rise in very sick people coming to hospital and action is taken to stop the spread, it takes 2 weeks just to see how bad it was when you started, and 2 more weeks to see the results of your attempts to slow it. That can be a long time to have no room in the ICU.
5- Those who do get unwell with COVID-19 tend to be sick for a long time. There are two manifestations of this. First is the long ICU stays and long time requiring a ventilator. Time needing mechanical ventilation for this infection is notoriously longer than in other respiratory illnesses, with a median of 2 weeks on a ventilator in several studies. This makes the virus a disproportionately heavy burden on health care systems. That means compared to another disease with a similar hospitalization rate, COIVD puts more pressure on the system because those coming into hospital need to stay there longer. Secondly is the COVID “long hauler” syndrome. Still little understood, this describes the significant number of survivors who are left with some level of functional disability lasting for a prolonged period of time, with some still suffering indefinitely since their infection. We still don’t know how long these symptoms might last. About 10% of those infected experience some form of prolonged illness. It occurs in people of all ages, and even in those who only had mild symptoms during their initial infection. Due to a propensity to increase the risk of blood clots, COVID infections also cause a disproportionate rise in life or ability threatening strokes, heart attacks, pulmonary emboli and other viral inflammatory complications. Lives can be ruined even in survivors.
THE BATTLE
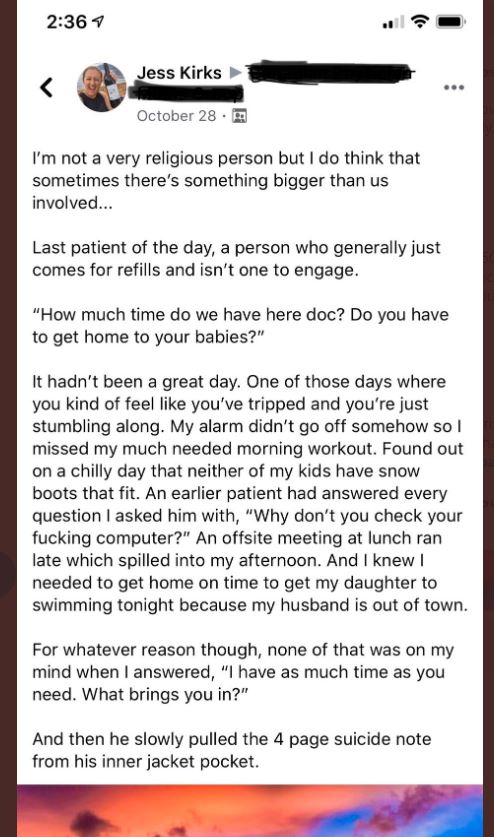
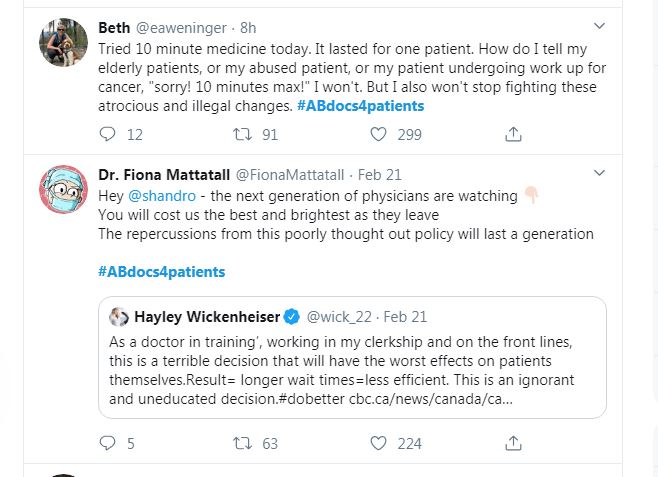
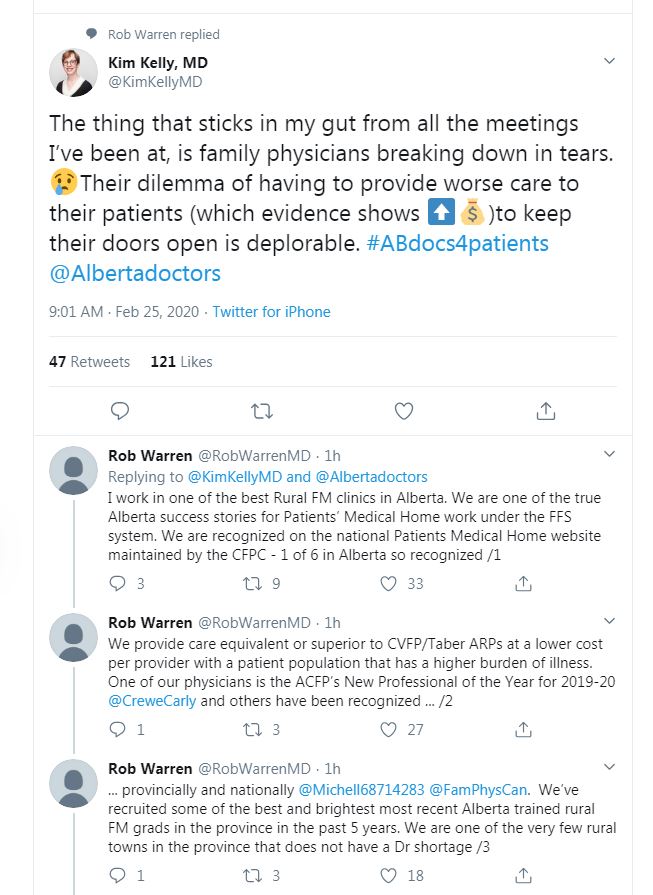
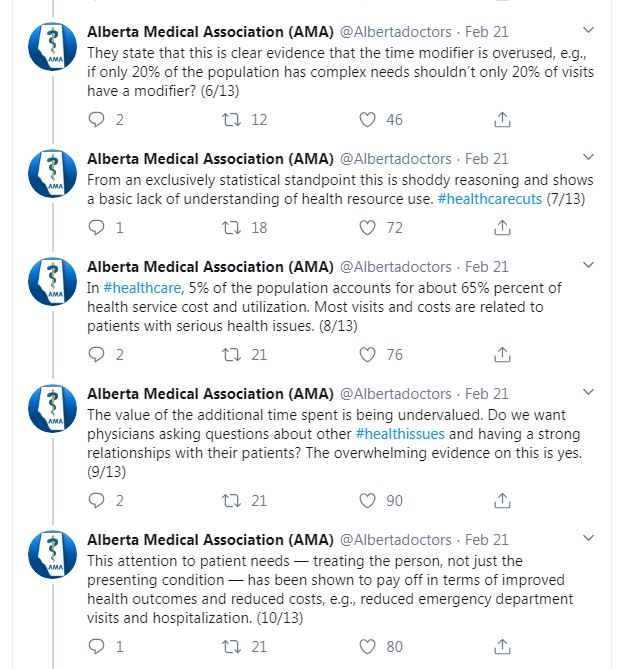
That’s it really. It’s those 5 features of the virus introduced into a naïve population (meaning one without any pre-existing immunity), combined with modern global travel patterns and the structure of our health care systems that can explain almost all the unique challenges of this pandemic. In the absence of testing and interventions to control it’s spread, it has followed the same pattern in many places. It enters a population silently, and begins rapidly spreading through asymptomatic or mildly unwell individuals. That 1 – 2 week cycle between infection and illness can be repeated several times without much notice, as most people are not getting very sick, and those who are going to eventually be very sick do not become so right away. By the time the trend of increasing illness gets onto the public health radar, there is already a high level of community spread, and many more people who are on the cusp of severe illness. This was the hallmark of early pandemic experiences at hospitals in places like China, Italy, Spain and New York that raised the alarm for health care workers around the world. And it was health care workers speaking out first. Days to weeks before COVID-19 began to dominate headlines, it was filling my med-Twitter feed with posts by concerned caregivers throughout the world. The warning was stark: first you don’t see it at all, then you see a trickle of mildly ill people, then you are crushed by a wave of the severely ill that keeps on coming. At this point, even if you implement strict public health measures, it takes another 4 weeks before your actions today will start to lessen that crush of sick people that is just starting to come in. This is how health systems have become overwhelmed. The crush is reliably followed a few weeks later by overwhelming demand for morgue space, and other body transportation and storage services.
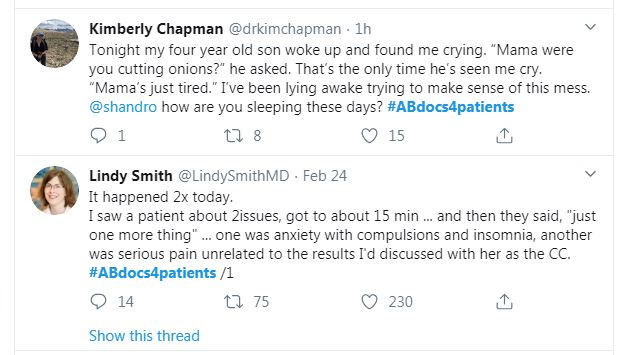
Let’s look more closely at what we mean by an overwhelmed health care system- or more correctly, an overwhelmed critical care system. It might be surprising to know how few extra very sick patients it takes in a given hospital to overwhelm its resources. Many are running on the edge (or just over) capacity in any given normal influenza season. Intensive care is exactly that- intense; it requires a lot of people and resources. It’s much more than just a bed and a ventilator- it’s all the doctors, nurses, respiratory therapists and other health care team members needed to care for the patient. There is a good deal of specialized training required to know how to do this. You can’t just throw any doctor or nurse in the ICU and expect they are going to be able to provide the best care. Overflow can be dealt with to some extent, but only for so long. Staff become burned out, or exposed and infected themselves. The COVID-19 death toll among health care workers is sobering. People have often been brought in from elsewhere- which can only happen when there are places with people to spare of course. COVID patients may begin to overflow into other units and critically ill people may stay in the ER longer than they should. All these resources turned towards pandemic patients need to come from somewhere. This blocks critical care beds and staff from the usual, routine needs that are still there: trauma, heart attacks, strokes, sepsis, overdoses, recovery from critical surgery, and all other forms of critical care are affected in an overwhelmed system. It can become impossible to provide the normal standard of care for a host of medical problems. Not to mention the difficulties presented by all the PPE staff must wear and work in. If you think it’s hard to order coffee through a mask and plexiglass shield, try working a multidisciplinary cardiac arrest wearing a mask, face-shield, a gown made out of a rubber shower curtain and still maintain good communication with people inside and outside a sealed room. All these factors increase the risk of substandard care and can inflate both the COVID death rate, and the rates of death or lasting harm from every other medical need requiring critical care.
This is the situation that health care providers, public health officials and concerned governments around the world have been trying hard to avoid for the past year. Success has varied from place to place, and time to time, but it has been widely agreed that it is unacceptable to allow health care systems to become so vastly overwhelmed that the death rate from otherwise survivable COVID soars, and that anyone needing hospital care for any reason becomes at risk of not being able to get it. This is the rallying cry to “flatten the curve;” it is to smooth out how many people become infected in a given amount of time so the system can cope. If it seems like it’s taking a long time and repeated interventions to flatten, that’s rather the point. If it seems like you are making a lot of sacrifices for an overall death toll in your area that is sad but not terrifying, that is also the point. The alternatives are to try to completely eliminate it (with the most extreme public health measures, as has been largely achieved in places such as New Zealand and several Asian countries), or to let it “flame out” as quickly as possible, permitting the system to be overwhelmed for a time in the hope of achieving early herd immunity. Both these approaches take a view of getting over the pain more quickly; one the pain of a lockdown, the other the pain of the virus. The hope in each case is to limit the overall damage, albeit with a vastly different perspective on what is more important to protect. Jurisdictions that have opted for the fast flame method have generally reversed course after finding the cost and difficulty to be too high (Great Britain, Sweden), and seeing that it really hasn’t ended the problem any quicker. There is a lot of experiential evidence suggesting countries that pursued the elimination strategy successfully have suffered the fewest infections, least economic damage and shortest disruption to normal life. They are currently living with the lowest levels of pandemic restriction in day to day life.
This is a good time to point out that when we talk about interventions to protect the health care system, we are really only talking about a subset of infected people who are the problem: those who are sick enough to need the hospital, but strong enough that they have a chance to recover with medical care. This does not include the group with the highest risk of death- the elderly and the very infirm. Keeping someone alive through a devastating illness is not a trivial matter. It means taking over a number of the body’s failing organ systems, sustaining life and providing the body with time and resources to help it overcome an infection and heal enough to resume it’s own life sustaining functions. If the body is unable to recover despite this care, there is little further we can do for it. This is why the very elderly and those with very poor baseline health are often not even offered life support/ICU care. In some people this care is futile, as the body is not going to be able to recover from a severe illness, regardless of the care we provide. That’s when medical care becomes focused on end of life comfort. Everyone has seen the statistics showing those 80 and over are at highest risk of death from COVID. Yet in this US study (as one example) the median age of COVID ICU patients was 64, with only 22% of them aged 75 or older. This means a very large percentage of covid deaths are among those who were never treated in an ICU because such care would have been futile, or against their desires for a focus on comfort and dignity near the end of life. Covid ICU patients are for the most part those who are somewhere between middle age and recently retired; people who may have a comorbidity (most commonly diabetes, hypertension and obesity), but were otherwise living normal, functional lives. These are the “salvageable” potential COVID deaths that require an intact medical system to save.
Faced with this specter in the early stages of the pandemic, with incomplete information on how the virus spread, how high its true mortality rate was, and a limited ability to test for it, the best course of action was an abrupt and complete as possible shut down of much of society. Initially this was to buy time to develop tests, study the best treatments, ramp up production of PPE and medical supplies, implement pandemic capacity plans, and figure out how far the virus had already spread. When you have a pathogen that can spread so insidiously, with carriers unaware and a long incubation period, the only way to fight it initially is to change people’s behavior to deny it the opportunity to spread. In fact, until vaccination is widely achieved, this still remains the best way, which is why it has been so difficult to find a way to move beyond that heavy handed approach. Hence the cycles of quarantine/lockdown- both terms used rather nebulously over the past year to refer by most to the various rules, restrictions and recommendations designed to (or at least intended to) limit the amount of person to person contact through which the virus spreads. People are prone to argue whether or not lockdowns “work,” by which presumably they mean work in limiting the spread of COVID. How effective any single intervention is, and its trade off cost is a very valid discussion. However, the underlying intention behind such interventions is a sound principle that does work; anything that reduces how many, how often and how long people are gathered in close enough contact to share a respiratory virus with people outside their household IS going to slow, and could ultimately stop the spread of the virus. Further data over the course of the pandemic has confirmed that the highest risk “super-spreader” scenarios are large groups of people, indoors, unmasked and in close physical proximity for extended periods of time, as is reflected in the current CDC prevention guidelines. To the extent we limit or stop that from happening, we will slow the spread of COVID.
In fact, we have seen astounding evidence at how effective this is in other circulating diseases. You have no doubt heard the incredulous reports that there is little to no influenza (the flu) circulating this year. (And yes, we’re still testing for it. No the flu won’t make a COVID swab positive, any more than having tuberculosis would give you a positive syphilis test). It’s not the only thing that is AWOL this year. Pediatric bronchiolitis, croup, even asthma exacerbations are all staples in the ER every winter, triggered by respiratory infections. Where I work, they are almost non-existent this winter and I have seen similar observations by physicians in many places. How many colds have you had in the past year? Contrary to conspiracy claims, this is not because we are arbitrarily relabeling everything as COVID. It is because these conditions are all caused by infectious respiratory viruses, and we are in the midst of a worldwide campaign to stop an even more infectious respiratory virus. Reduced travel within and between countries, limited social gatherings, compulsive hand sanitizing and mask wearing are all having the exact effect one would predict- stopping the spread of respiratory infections. In the case of influenza, it may well have been largely stopped in the Asian and southern hemisphere nations where we usually get our new annual strains from- areas that are generally doing a better job than North America at COVID control. In fact, in my opinion seeing how well COVID has still spread as much as it has in the face of current measures that have nearly eliminated the flu and other respiratory infections is an even greater indication of just how contagious it is. If we had done nothing, it would surely have hit us so much harder.
Accepting that reducing personal contact does reduce transmission, we can then rationally discuss what measures work better than others to achieve this, what the costs of such measures are in dollars, freedom and mental health, and who pays the price for either decision. Certainly the hodgepodge of variable rules, restrictions and exemptions experienced in any of a number of jurisdictions during the pandemic highlight that there is not always a lot of evidence based decision making going on, but rather a lot of best guesses, influenced heavily by individual opinions, financial limitations, and local political persuasions or lobbying. While the rationale behind the lockdown approach is valid, the devil is most certainly in the details. Any intervention is also only as good as the public’s compliance to it, which has certainly waned as the pandemic stretches on, leading to further discussions on the merits and ethics of education, enforcement, and the diminishing returns of repeated “shut-downs,” where a possibly less effective result is being paid for by a potentially diminishing pool of voluntarily compliant individuals. There is a cost to moving in either direction, and it is often paid by different people in each case. This is a classic demonstration of how interconnected we are. No man (or woman) is an island, and our choices in these matters always affect others around us.
The costs of pandemic control measures to individuals, businesses and society continue to be abundantly clear. Limits on personal mobility, isolation from friends and family, loss of opportunity in education, sports and recreation, mental stress, loss of jobs, collapse of small businesses, bankruptcy, domestic violence, delays in routine health care and elective surgeries, delayed cancer diagnoses- the fallout from these and more will be with us for years. The longer the pandemic drags on, the more it is going to “suck” because of all these things. Much of this is unavoidable. Even if we assumed that no mandated public health restrictions were imposed, much of the economic and isolation consequences of the pandemic would still be with us. When people are aware of an existential threat to their own health, and that of loved ones, they change their behavior to limit risk. When a community is in outbreak, many people will chose to stay home, and businesses that rely on mobility and mingling will suffer. These are self preservation and economic choices; both immediate income and future earning potential can be decimated by serious disease in a home- to say nothing of medical costs where insurance is inadequate. It is a false dichotomy to assume that in setting a pandemic policy we chose either health OR the economy. Likewise, a full focus on protecting everyone from infection will still have inadvertent health consequences as surgeries are delayed and medical appointments put off. There is no policy of pure health or pure economic protection- only compromises and priorities. There is evidence to support that the harsher short term economic and public restrictions of a viral elimination strategy actually do the least overall economic damage. If viral spread is successfully stopped and nearly eliminated early on, life can return to normal much sooner- albeit with significant surveillance effort to prevent a re-entry. The alternative, which most of the world is living with, is repeated cycles of opening and closing as cases and hospitalizations cycle, with no return to normalcy in between. Whether these closures are driven by government policy, or people’s natural behavior in the face of local flare-ups, the effect is often similar. And given the long incubation period, each part of the cycle drags on for weeks. Off and on half measures to live with this “slow burn” of cases leads naturally to the longest period of societal disruption and living with an ever present small to moderate risk of infection. Whether there is more suffering from prolonged restrictions, or more suffering from viral infections and deaths varies from place to place and is perhaps a matter of personal perspective.
SEEING IS BELIEVING
A prevailing theory in understanding the anti-vaccination movement is that vaccines are a victim of their own success. In a world where very few people have personally seen the effects of polio, tetanus, or even measles encephalitis, it becomes increasingly more difficult to remind people that these diseases exist, and that they are terrible. People become complacent, and question the need for vaccination. I suspect we are seeing a similar effect from the tenuous control we have achieved in much of the world over COVID. While the overall death toll still remains distressingly high, the fact that we have prevented the near simultaneous overwhelming of most of the world’s medical facilities that was feared in the early months means that most people’s entire experience of the pandemic has been the disruption of their lives from the policies and restrictions put in place to control it. They may see low local death tolls- a consequence of successful transmission suppression- and wonder what’s so bad about this virus. Combine that with how well we have isolated the sick, and the very common experience of having “mild COVID,” and it is not surprising to see doubt creep up about how necessary this all is. Certainly millions of families worldwide have personally experienced the tragedy of an early death of a love one, but maybe the very isolation that keeps us safe also prevent us from sharing with one another more intimately the reality of death from COVID. If you have not had someone close to you be very sick, or if you do not work in a facility that cares for them, then you will have little first hand knowledge of what is so bad about COVID. We live in a world where there are many voices trying to convince us someone is fooling us about any given issue. When it is so hard to see the damage for yourself, many people may find such claims about the pandemic to be a seductive path back to normalcy.
A part of this perception is certainly the striking regional variability that has been seen with “spikes” of covid. Parts of a country or even city can have much higher case loads than another, and the strain on the local health system can come at different times. This is likely a result of decreased movement between regions, but with the propensity for COVID to spread rapidly within a susceptible, localized population. If the virus gains a foothold in a care facility, a close knit neighborhood with poor distancing practices, or a homeless shelter with a large transient population, there can be a significant local spike in cases and hospitalizations. Super spreader events like weddings, funerals or house parties can make a noticeable difference to local health facility needs a few weeks down the road. Governmental restrictions or recommendations tend to be much broader than these local outbreaks, meaning you may be living under restrictions tailored for communities nowhere near yours. It’s also important to remember that an overwhelmed ICU can still exist in an otherwise underutilized hospital and primary care system. When critical care is overwhelmed, elective surgeries get cancelled, visitors are restricted and anyone who doesn’t need to be in the hospital is kept out. People self restrict their movements, so medical clinics may be empty, and ERs avoided except in the most extreme need. Remember not everyone in health care can provide critical care- those that do can be over-run with sick patients while the rest of us find we have much less to do than normal. If you are not in the ICU, the hospital can seem a surprisingly empty place at such times. It’s not going to look like a scene from an outbreak movie, or from Lombardy Italy in early 2020 unless things are seriously out of control. That’s the scenario we are trying to avoid.
The average person is not going to see the side of the pandemic that critical care providers, or nursing home staff are going to see. And that’s on purpose- the fewer people exposed to the environment of heavy COVID viral loads, the better. Likewise it is fair to say those in health care and political decision making are sheltered from the most severe economic impacts compared to those who are losing their jobs or businesses. I will mention that is not universally the case- as surgeries are put off, clinic visits reduced, and even routine ER visits tumble, there is probably an overall loss of income that has been experienced by most of the health care community this year, at least where I am from. Yet, that is not the same as businesses that can no longer open, or employees who’s service based skills are no longer in demand. There is also the important consideration of those working low income labor jobs who do not have the economic luxury of staying home, even when sick. Working conditions often come with their added risks too. There is a reason there have been so many large outbreaks linked to meat packing plants. No plan for the sick or exposed to take a mandatory leave of absence is going to work if the financial support to make that possible is not provided. It is important for all of us to consider the perspective of those experiencing a very different pandemic than we are.
IS THERE A BETTER WAY?
That’s what everyone wants to know, and I don’t have the knowledge or qualifications to give the answer. There are a lot of popular and attractive ideas out there. Some give simple, painless sounding (or at least less painful) solutions that they insist are better. As in all complex problems, I fear many simple solutions are too simple, and gloss over some of the realities of this pandemic. We can look at them too through the lens of understanding the unique properties of SARS-CoV-2.
One popular approach advocated in the Great Barrington Declaration and similar proposals is to simply protect the vulnerable, get on with our lives, and wait for herd immunity to take hold, presumably after everyone young and healthy has been infected and recovered. It’s a nice idea, but if you try to develop a specific policy based on that, while keeping in mind the insidious and stealthy nature of the virus, it loses its simplicity. Who are the vulnerable? The elderly for one- do we simply lock them away with no outside contact? No visitors, no leaving home? Are we not already essentially doing almost that and still seeing regular stories of terrible outbreaks and death in senior facilities? And this is while we still have all these other rules and restrictions on for the general public. Where do they go for medical care? Who takes care of them in their facility? Do we also make caregivers live in the facility with no outside contact? What about their families? How often do we test everyone? The tests are imperfect, and false negatives are the most common error. What do we do when a case slips through? What about those not in a senior facility already? Do we build massive complexes to house them in? Are they allowed to stay at home or with their families? If they do, are their families allowed to work or leave? Maybe you don’t want to impose rules, so everyone “voluntarily” decides how they are going to protect their relatives. How can they do that when anyone they meet could potentially pass on the virus without warning, and they themselves could be unknowingly infectious for the next week or two? It’s a false choice- there is no real action they can take to protect their loved ones without completely isolating themselves from society. Who else is on the at risk list? There’s the immunocompromised (including cancer patients and those on immunosuppressive drugs for many different chronic diseases). People with high blood pressure, diabetes, obesity. Pre-existing respiratory conditions. There is no firm line between high risk and low risk- there is a spectrum and it is very hazy at points. What policy do you make that is going to realistically allow those at high risk to stay safe while letting everyone else carry on with life as normal? There isn’t one- you can’t do it. Even the blanket shut-downs many of us have been living under (which are entirely un-necessary according to the Barrington philosophy) are not enough to adequately do this.
The entire question of whether or not herd immunity can be achieved through natural infection is another issue. I won’t delve into it, but there is mounting evidence that natural infections may not provide the complete long term immunity that would be needed for this to work, at least not for enough people. We also know this virus mutates easily. Every new host is another opportunity for mutation, and any new mutation could be the unlucky one that raises mortality, increases infectivity, and evades the old immune response. There’s a very good chance if you let if “burn through” the population that the virus that comes out on the other side will be different enough to start the whole infection cycle over again. This is the same phenomenon by which we have new flu variants every year. Furthermore, with uncontrolled community spread (even somehow sparing the elderly and infirm) there would also not likely be a way to prevent prolonged overburdening of the health care system, which as described above will increase all cause mortality. Remember, the ICU system is there to support mostly the middle age to retirement age group who are the infection deaths potentially preventable through good medical care. There would be a large sacrifice in this age group too with this approach (and certainly some even younger too). Alberta Health Services put out a very fair and comprehensive discussion of some of the limitations of the Great Barrington Declaration.
So what about elimination? It has been done very well in several nations where people are living a mostly normal life today. Can other countries, states or provinces go for COVID zero? Perhaps. I don’t think there is any theoretical reason it could not be done, and the evidence certainly suggests that it is the least painful and quickest path out. There is an argument to advocate for it in Canada, in light of the new variants beginning to spread more widely. If you are not an island there are certainly more travel complexities to address, but I think the biggest barrier is public buy in. It won’t happen if most of the public is not entirely on board with the true, real and significant lockdown that would be required to get there. Even with the promise of “normalcy” afterwards. Even if a western government was willing to impose such a program against the will of a part of the populous, it would not be enforceable. Maybe at the beginning of the pandemic there would have been more appetite for it. If we knew how long it would drag on, I think there might have been in many places. But here in the west we have generally been given political messages of overly-optimistic reassurance with too early reductions in restrictions, and inadequate travel rules to keep new cases out, and existing ones from spreading. A more realistic comparison to the multi-year phases experienced in all prior pandemics may have made the prospect more attractive. I would support the attempt, but I don’t see it happening now, especially with vaccinations beginning (even though that too will take a long time to significant herd immunity).
THE WAY OUT
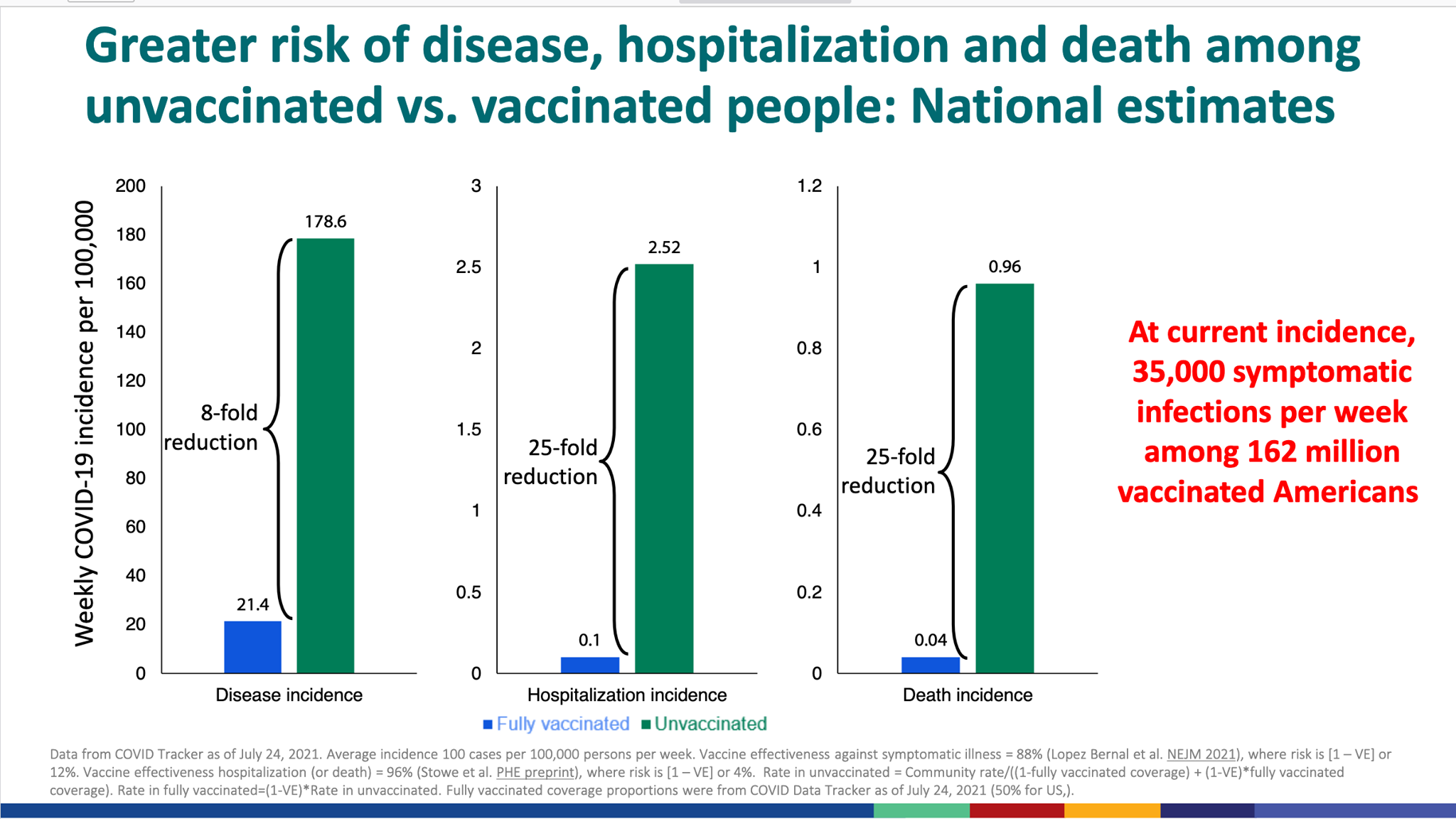
Clearly there is no quick and easy path out of the pandemic. Whether we double down in squeezing it out, or give up and let it run rampant, there is pain in either direction. There is hope in the excellent clinical data and evolving real world experience with all the major current vaccines undergoing distribution. Mass vaccination is I think the best way out, but it will take time and public buy in. If you are frustrated by wearing masks, not seeing family, and an inability to work or travel, this is certainly the fastest way back to normal. Get vaccinated when you are able to. It is safe and effective. Most frontline healthcare workers where I live have already gladly received it. The longest, and most painful path is to deny the virus is a threat and help keep it burning right on the edge of overwhelming the critical care system by refusing to follow the basic health guidelines that have been given. They only work if they are followed, and if they don’t then we either enforce more painful restrictions until they do, or give up and surrender to the virus. There is at least now an endpoint on the horizon.
As I’ve said before, there is a valid discussion to have about what interventions, rules and public health measures are most useful, and which have a greater cost (economic, personal or otherwise) than they are worth. If we are to continue on the path of the slow burn until herd immunity by vaccination, then we must continue to be diligent and cooperative, and accept that things will not return to normal until that point. If we acknowledge both the reality and the risk of the virus, as well as the cost of the measures we take to control it, we are better able to make wise decisions. There continue to be challenges ahead, particularly with new, more infectious variants staring us in the face. We will also continue to learn more about the virus, and the success (or not) of different containment measures. We should be willing to alter our course based on new information, and that information- as well as its limitations- should be freely shared with the public.
The COVID-19 pandemic is a major challenge to our society- no secret plots or conspiracies necessary- it’s the nature of the virus. It’s not the first such challenge to humanity, and not the last. I’m not going to claim there are not people who are using this as an opportunity to further their own political agenda, or to profit economically from the suffering of others- these things have always been with us, and in the increasingly hyper-partisan political world of the west, will continue. The media loves sensationalism and will focus on what catches the most attention, as they too always have. But there is still plenty of good and objective reporting behind the hype of headlines and sound bites, and there are plenty of civic and medical leaders trying to find a path forward where there is no clear best answer. Hopefully a little more understanding will motivate people to spend less time looking for hidden agendas, and more time discussing the legitimate and difficult questions of how to live with this reality. How do we balance saving lives with restricting personal liberty? How do we protect health care systems from becoming overwhelmed without causing irreparable economic harm? How can we make it more financially possible for people to isolate when they should? How do we make these decisions when we still have incomplete information about the spread of viral variants and the best ways to contain them? These are not simple questions and are worthy of tough discussion. But when we are distracted by false information, unyielding conspiracy theories, and the need to constantly defend the utility of scientific expertise, then we cannot even have these discussions. Let’s acknowledge that this is hard on everybody, and we are all doing our best. Opinions can and should differ, but we can still do our best to make sure we are using real information to make really important decisions.